A 25-year-old Venezuelan male presented to a Chicago area emergency department (ED) in early November 2023. He had traveled with his family through Panama, Costa Rica, Nicaragua, Honduras, Guatemala, Mexico, and Texas before arriving in Chicago approximately one month prior to his ED visit. He noted spending about five days walking through a jungle, as well as traversing rivers. This was his third presentation to an area ED for the same complaint of a right forearm wound. It was initially treated with trimethoprim/sulfamethoxazole and cephalexin with no improvement. It was slightly painful but not pruritic. On presentation, a 4-cm wound was noted on his right forearm [Figure 1]. His daughter had two similar lesions on her right leg [Figure 2]. He also had multiple nodules along his forearm. The wound had been worsening for the last three weeks despite antibiotic treatment.

FIGURE 1: Right forearm wound at time of third ED visit (tattoos distorted for privacy). (Click to enlarge.)
There was concern for possible cutaneous leishmaniasis (CL), therefore he was admitted to the hospital for infectious-disease and surgical consultations, as well as to complete a punch biopsy the following day. He was discharged with followup at an outpatient wound care and a primary care clinic. Biopsy results were available to the care team 20 days later (after being sent to a Mayo Clinic) with confirmation of diagnosis of CL. At this time, consultation was made to infectious disease specialists, as well as the ED pharmacy team for assistance with treatment options. The patient was uninsured with limited resources, making miltefosine cost prohibitive. Paromomycin cream was not available in any local or regional pharmacies. The components for paromomycin cream are not FDA approved and are sourced from outside the U.S. on a case-by-case basis and sent to a compounding pharmacy in the area on behalf of the patient. The patient was able to receive the paromomycin cream from the compounding pharmacy, and has been following up with wound care. He is noting slow improvement in his wound.
What is Leishmaniasis?
Leishmaniasis is a vector-born protozoal disease transmitted by sand flies, considered to be endemic in 99 countries.1 Texas and Oklahoma have endemic levels of CL, but there is no endemic level in the northern United States.2 Globally, cases are most common in the Middle East, North Africa, Central America and northern South America. There may be 700,000 to 1.2 million cases of CL per year globally; however, CL is not a reportable disease to the CDC, so there is no reliable way to track U.S. cases.3 Historically, most cases diagnosed in the U.S. were related to military travel and deployment, with a few cases related to leisure travel. Leishmaniasis is an obligate intracellular parasite in mammals with an incubation period of weeks to months. CL is a spectrum of cutaneous disease ranging from localized to diffuse which result in ulcers, but no mucosal involvement.4 Leishmaniasis can also present as mucosal leishmaniasis (ML) and visceral leishmaniasis (VL) with ML being a metastatic sequela of CL years to decades later. VL is generally an acute process, incubating for weeks to months causing fever, weight loss, hepatosplenomegaly, pancytopenia, and an elevated serum protein level.5
Conventional treatment for CL involves local topical treatment or systemic treatments. There is one parenteral treatment approved, amphotericin B, which is highly toxic and generally reserved for severe cases of diffuse disease or visceral leishmaniasis. There is one oral treatment that is FDA approved, miltefosine 50 mg three times daily for 28 days. A full course of this medication costs approximately $60,000. There are topical medications, paromomycin and pentavalent antimonial (SbV) compounds, available in other countries, but none has been approved by the FDA.5 It is possible, although challenging, to get these medications through compounding pharmacies in the U.S.
Discussion![]()
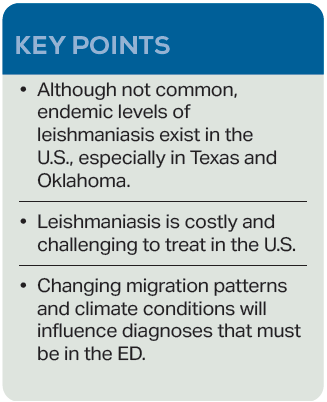
As the refugee crisis continues, and asylum seekers visit emergency departments all over the U.S., physicians will be exposed to pathologies we may have only heard about in medical school. Climate change will also influence the prevalence of CL and other conditions traditionally considered tropical diseases. This is from a combination of human migration patterns and the expansion of climate conditions in which the sand fly vectors can survive.6 Currently, climate models estimate that 12 million people live in locations in which leishmaniasis is endemic in the U.S. Because of no required tracking or reporting, we have no accurate measure.7 This case emphasizes the importance of maintaining a wide differential, especially when evaluating asylum seekers who have been exposed to a wide variety of environments and pathogens. Our local infectious disease specialist estimates that the last time a case of CL was seen at this hospital was at least 15 to 20 years ago.
 Dr. Englof is current faculty of the Swedish Hospital Emergency Medicine Residency (part of Endeavor Health) in Chicago, and a program coordinator for EMGLEX, an immersive emergency medicine rotation for international physicians.
Dr. Englof is current faculty of the Swedish Hospital Emergency Medicine Residency (part of Endeavor Health) in Chicago, and a program coordinator for EMGLEX, an immersive emergency medicine rotation for international physicians.
 Dr. Dupont is a second-year emergency medicine resident at Swedish Hospital in Chicago.
Dr. Dupont is a second-year emergency medicine resident at Swedish Hospital in Chicago.
References
- Ruiz-Postigo JA, Jain S, Madjou S, et al. Global leishmaniasis surveillance: 2021, assessing the impact of the COVID-19 pandemic. Weekly Epidemiological Record. 2022;97(45):575-590.
- Curtin JM, Aronson NE. Leishmaniasis in the United States: Emerging issues in a region of low endemicity. Microorganisms. 2021;9(3):578.
- Centers for Disease Control and Prevention. Leishmaniasis – Epidemiology & risk factors. CDC website. Last reviewed February 18, 2020. Accessed January 15, 2024.
- Convit J, Ulrich M, Fernàndez CT, et al. The clinical and immunological spectrum of American cutaneous leishmaniasis. Trans R Soc Trop Med Hyg. 1993;87(4):444-448.
- Centers for Disease Control and Prevention. Leishmaniasis – Resources for Health Professionals. CDC website. Last reviewed October 5, 2023. Accessed January 15, 2024.
- World Health Organization. Leishmaniasis. WHO website. Published January 12, 2023. Accessed January 15, 2024.
- Barnhart, M. A ‘tropical disease’ carried by sand flies is confirmed in a new country: the U.S. National Public Radio website. Published November 1, 2023. Accessed January 15, 2024.
The post Case Report: Cutaneous Leishmaniasis in Chicago appeared first on ACEP Now.